Alzheimer’s affects a staggering two-thirds of the UK population. Let’s let that sink in for a moment… and no it’s not limited to the elderly! With this month being Alzheimer’s awareness this month, we want to stress how imperative inclusion is to this disease. Not only to those suffering but the amazing caregivers supporting them.
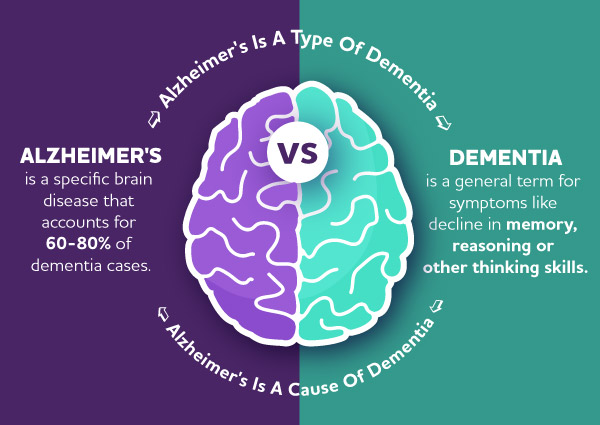
Alzheimer’s VS Dementia
So, what is Alzheimer’s and how does it differ from Dementia? Dementia is not a specific condition; it’s an umbrella term for the symptoms of a decline in brain function. Alzheimer’s, on the other hand, is a specific type of disease and a common cause of dementia.Alzheimer’s involves the progressive damage of brain cells, which messes with things like memory, thinking and other mental functions.
In the UK, Alzheimer’s is responsible for six out of ten cases of dementia. The second most common form of dementia is vascular dementia, followed by Lewy body and frontotemporal dementia. These names are given depending on which area of the brain has been affected, shedding light on the different ways dementia can affect people.
Alzheimer’s usually starts with memory issues, like forgetting recent events and struggling to pick up new information. But as Alzheimer’s progresses, it involves further difficulties such as memory loss of daily activities, speech difficulties, less ability to focus, feeling lost, mood swings, increased anxiety and sometimes even increased aggression.
 Credit: Alzheimer's Association
Credit: Alzheimer's Association
What’s Your Brain Age?
It is true that Alzheimer’s symptoms usually show up around the mid-60s and beyond, at least in most cases. But here’s the thing, there is a big misconception that dementia is a normal part of getting old. Well, it’s not! Sometimes, younger generations fall into an ageist thinking trap, and it’s all because of stereotypes about ageing.
Unfortunately, younger generations tend to stereotype elders as being mentally slower, physically weak, not open to learning new things, stuck in their ways, grumpy, and dependent on others, among other things. We’re all guilty to some degree of cracking jokes about memory or hearing loss and normalising a culture that’s all about anti-ageing.
However, it’s crucial to recognise that Alzheimer’s does not exclusively affect the elderly; it can impact people of all ages. Alzheimer’s can show up as early as your 30’s or 40’s, and when it happens before the age of 65, it’s called ‘early-onset Alzheimer’s’. In the UK, about one in twenty dementia cases falls into this ‘early-onset’ category. So, while it’s not super common, it’s still important to understand that this condition can affect anyone.
Gender Gap
Now let’s talk about gender: globally, dementia affects women more than men, outnumbering men two-to-one in cases. Even more shockingly, Alzheimer’s is currently the leading cause of death among women in the UK. But why is this gender gap happening? Well, age plays a big part because, women tend to live longer than men, and that’s why we see more cases among women. But our life experiences can also contribute to a higher dementia risk. Biological factors, such as menstruation, pregnancy and the menopause in particular, may be increasing the risk when it comes to dementia.
However the gender gap may begin to close, as cognitive reserve plays a big part in potentially delaying dementia. The more we use our brains throughout or lives the bigger the reserve (use it, or lose it!) Women have historically had more mundane tasks in their gendered roles with mental stimulation not readily available. Whereas their male counterparts have had more opportunity for higher education, career advancements and continuous stimulation in their day to day tasks. So as stereotypical gender roles dissipate the chances are so will the gap in Alzheimer’s.

Race Against Time
Another aspect that often gets overlooked is Alzheimer’s in ethnic minorities. In the UK, BAME (Black, Asian, and minority ethnic) communities make up just 3% of dementia cases, which is roughly around 25,000 people. However studies show that this could just be an under-capture in data, due to the delay in diagnosis within the BAME communities. In actual fact black people have been proven to be at 22% higher risk than white people, while south Asian’s are reported to die sooner after diagnosis. Truth be told there’s a wealth of stats out there and all the data is different depending on the factors of the studies. However they all seem to boil down to one conclusion; more needs to be done to make Alzheimer’s and dementia care accessible for minority ethnic groups.
South Asians & Alzheimer’s
From faith and cultural practices which deter seeking westernised medicine to language barriers (dementia translates to: insanity or of unsound mind in Urdu) South Asian’s have a hard time with the acceptance of Alzheimer’s and dementia. Within their community it can be seen as taboo or have a stigma attached. Many religions put a huge emphasis on taking care of your family. So, seeking external assistance might make them feel like they’re falling short on their familial duties or taken as a sign of weakness.
So It’s easy to see why there’s a higher percentage of late diagnosis. However it’s what can be done about it that needs to be addressed. Memory tests performed by GP’s as a first step in diagnosing Alzheimer’s are aimed at the white population. Altering these tests to be conducted in a patients first language and be applicable to their culture may yield more accurate results and in turn an earlier diagnosis. Educating the community with outreach programmes to destigmatise, and representation are all key in making Alzheimer’s care inclusive.
Higher Risk
The black community, however have other barriers and inequalities when it comes to Alzheimer’s. The data may show that BAME groups are less prevalent but there are some pretty big discrepancies when you compare diagnosis stats. So, can the numbers be trusted? What they do show however is that the black community though under-diagnosed may in fact be more pre-disposed to contracting Alzheimer’s. This is due to genetic and other health factors. Black people are at a higher risk of vascular disease, diabetes, obesity and lower socioeconomic backgrounds which are all risks of developing Alzheimer’s or dementia.
Like south Asians and other minority groups black people are also likely to get a late diagnosis. This is in part due to the individual’s reluctance to seek help. Black women in particular are known for being strong matriarchs. They often put aside any health concerns as they don’t want to be seen as a burden to their families. The other side of this is the misconception within the black community that memory loss is a natural process of ageing.
It has also been recorded that black people with Alzheimer’s tend to experience the symptoms more severely. And are more prone to hallucinations and delusion. This leads to being over prescribed with antipsychotic drugs that can have serious side effects… Including an increased risk of death. This is just one area where the level of care for black people with Alzheimer’s is questionable. Black people in care homes are often overlooked or their needs are not met adequately. For instance, the hairdressers brought into care homes aren’t trained in dealing with Afro hair. Though a small thing to some, it’s those small things that make black people still feel segregated.
Dementia doesn’t discriminate
After looking at all the stats, risk factors, gender and racial disparities. The percentage of people that are affected by Alzheimer’s or dementia whether directly or indirectly is huge. And with under diagnosis being rife it’s probably bigger than we can imagine. What we can ensure is that everyone is aware of the symptoms, the lifestyle factors that we can change to try and delay or prevent, and the level of care and support offered.
Yes, Alzheimer’s and dementia may be more prevalent in women, older people and black people. But overall it can and does affect anyone and everyone regardless…you could even say its inclusive. And that is exactly what we as a society and the health care system need to be.
From diagnosis to clinical and community care more needs to be done to support patients and their families. Everyone should have the best quality of care and lives they can whilst battling with this incurable, heart breaking disease. It’s not just the health system though, we as a society need to not write off our elderly as senile. We need to be aware, be more patient and help lessen the stigma.
Sometimes Alzheimer’s and dementia can be seen as regression and it may be easy treat those affected like children. But they’re not kids, they lived a life before us, they’re the ones that paved the way for us. They deserve to live all of their days with dignity and respect, not belittlement.

Respite, Resource and Inclusion
For loved ones turned carers, Alzheimer’s and dementia can be a particularly difficult disease. Imagine how it feels, when it seems the person you used to know has faded away. They may have even forgotten your name, or become hostile towards you. And as their moments of lucidity become less frequent it can not only be soul destroying but isolating. Which again is why inclusion is paramount!
Isolation isn’t good for anyone, we’ve all learned that in recent years, thanks COVID! Including Alzheimer’s suffers and their carers within the community can make all the difference. It can offer respite for the families and carers but it can also alleviate some of the symptoms of Alzheimer’s. We’re social creatures by nature, so offering safe spaces and opportunities for them to interact can be enriching for all.
There are a wealth of resources available if you’re affected by Alzheimer’s or dementia. Even if your not now, the odds are at some stage you will be. Whether that be yourself, or a family member so get Alzheimer’s and dementia aware now. After-all, it all adds to your cognitive reserve!
